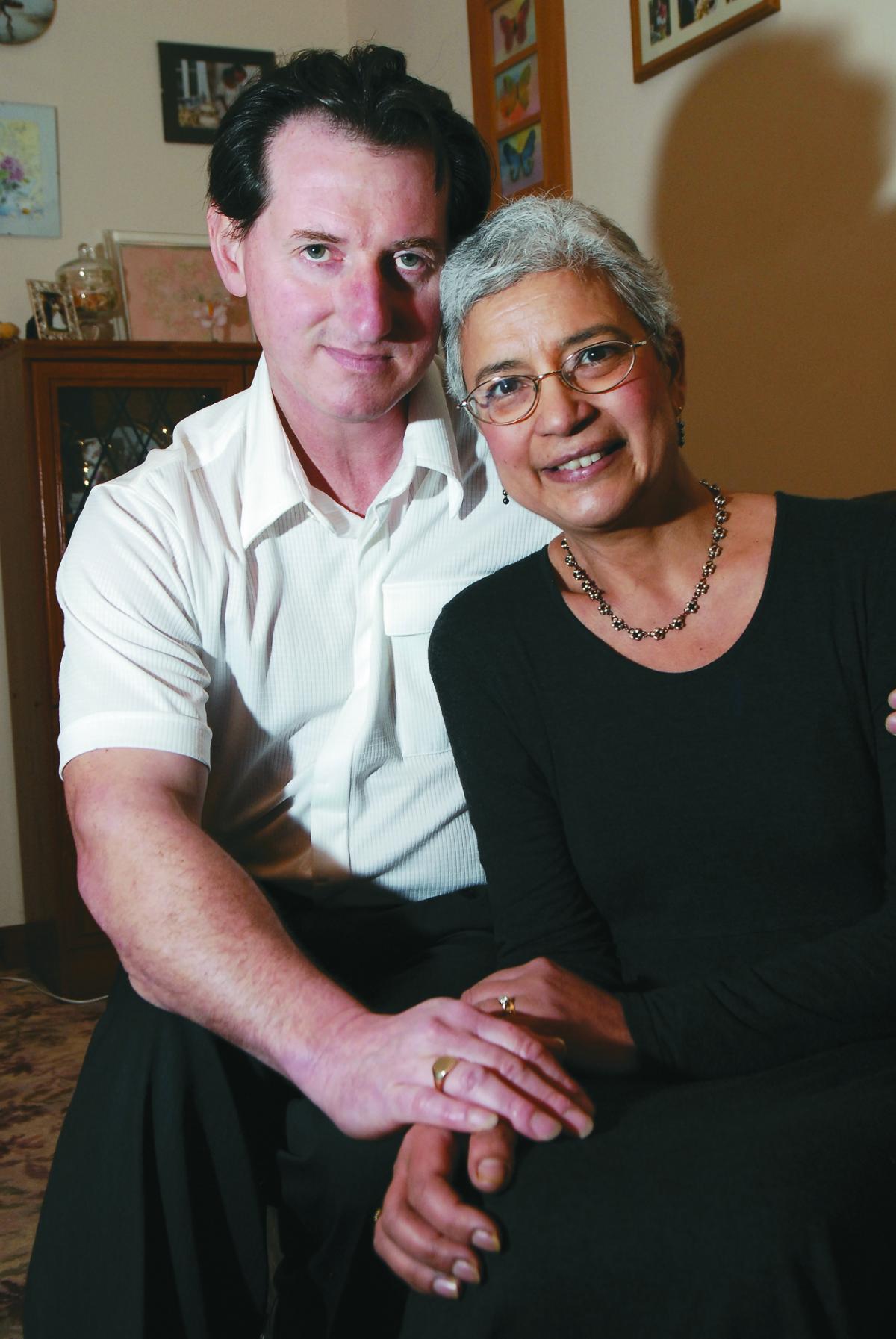
RETIRED Worcester teacher Barbara Moss is on a compelling mission which she finds really exhilarating. This is great news and not exactly what you would expect from a woman who was given just three months to live nine years ago.
Facing the devastating news in 2006 that she had inoperable stage 4 – the final stage - bowel cancer (known as colorectal cancer or CRC) which had spread to her liver, she discovered the drug she believed could save her life was unavailable on the NHS.
But Barbara, a former teacher mainly of English at Blessed Edward Oldcorne RC Secondary and the Royal Grammar School, drew on an inner resource – will power – to survive and recover.
She started looking on the internet and researching available treatments. The drug Avastin was the one she felt was her best hope but, when she asked for it, she was told she could not have it on the NHS.
The mother of two, from Aconbury Close, Worcester – ironically a few yards from Worcestershire Royal Hospital – decided to pay for her own treatment from her pension. The total cost was £21,000 - £4,000 for the drugs and the rest went towards paying for the time of nurses and consultants, provided free to other NHS patients.
Because she paid for her so-called “top-up” drugs privately, she lost her right to free NHS care from the system she had paid into all her working life.
“I did take a certain amount of risk,” she admits. But it certainly paid off and she has no doubt that Avastin saved her life. Her cancer shrank so rapidly that it became operable and the tumour was removed at the Queen Elizabeth Hospital in Birmingham a year after being diagnosed.
Her battle with cancer did not end there and she has regular check-ups she says: “I still remain cancer free, now nine years on.
“I did have some worries earlier this year when my tumour marker indicator (CEA blood test) rose progressively three times above the normal levels. This reading is still out of normal right now but I feel fine.
“I feel assured because I have received all the checks available, a CT scan, a CT/PET scan and a colonoscopy, all of which were clear.”
Barbara’s experiences inspired her to try and do something about what she felt was an unfair system of denying people life-saving treatment on the NHS and has been campaigning for greater access to cancer drugs on the NHS ever since.
“I felt it was really unfair and I felt I had to do something about it,” says the 61-year-old.
And this tireless campaigning, which has expanded to the issues of involving patients in decisions about their own treatment as well as their consultants, has resulted in an action-packed 12 months for Barbara, and her husband Mark, as she has spoken at different events in the UK and Europe and before eminent medical professionals and politicians.
She says: “There is a fantastic leap forward in the treatment of cancer, including colorectal cancer, and it is so exciting to be involved in this right now. The patient experience is invaluable in assessing the value of a drug, not just for its effectiveness but also for its tolerability and side effects.
“Mark and I have been in a number of areas, both at home and also in the EU. Cancer is treated so differently today. Basic chemotherapy kills all dividing cells but personalised medicine means that you are tested to see what treatment you are likely to respond to so you are not given treatment that cannot possibly work for you.”
She believes the NHS 100,000 Genomes Project is the world leader in sequencing the genomes of 100,000 patients and this is a breakthrough for the treatment of cancer as well as other rare diseases. She is hoping to become involved in this in the spring at a patient expert level.
“In 2015, I was involved with many different groups. At the beginning of the year, I was asked to present an opening talk for the launch of a major new clinical trial by Roche in Holland.
“I was humbled to be speaking to so many people of high intellect - researchers, oncologists and doctors. They were so appreciative to see the results from the patient’s side and it gave them a meaning for their work.
“In February, Mark and I were invited to the annual congress of a Dutch charity called Inspire2Live. The theme was ‘Breaking the Barriers for Patients’ and it was wonderful to be among so many inspirational people who truly wanted to make a difference in improving conditions for cancer patients.
“Shortly after, we were invited to two events in London - Beating Bowel Cancer’s Parliamentary Reception and an EU workshop at the London School of Economics.
“I am regularly approached by various organisations such as the European Medicines Association to advisory or licensing meetings for new drugs. I am patient ambassador for Bowel Cancer UK and also for Europacolon.”
Barbara also chairs a European Expert Patient Advisory Group (EPAG) and has written various documents for patients about CRC for the website. The group is planning a major survey on the unmet needs of bowel cancer patients where the cancer has spread to other parts of the body.
She was recently sent the Cancer Drugs Fund (CDF) 2016 proposals by the National Institute for Health and Care Excellence (NICE). This is a document and online public survey that are available to all. To see these proposals visit https://www.engage.england.nhs.uk/consultation/cdf-consultation/consult_view
“There are many proposed changes to the CDF 2016 with early access to drugs being very important. This is to be welcomed, but there are many conditions that are so complicated.
“I have written directly to many organisations which all find it confusing so I wonder how the general public is expected to respond by February 11. I am trying to find out more about this so I can advise others,” says Barbara.
She adds that her campaigning work is a very important part of her life. “I think it exhilarates me to be actively involved and to be able to talk to these people and put forward the patient’s point of view.
“It has captured my heart because I have seen the unfairness and it is about people’s lives and nothing can be more important. I find it very rewarding but I also find it compulsive – I feel I have to do it.”
Barbara also takes every opportunity to encourage people to live healthy lives by eating fresh fruit and vegetables which, she says, has been proven to prevent the incidence of cancer along with lowering consumption of alcohol and not smoking.
She also tries to encourage people to accept the screening invitation at the age of 60. Early detection gives people a better chance of successful treatment and cure without needing chemotherapy.
“Bowel cancer is occurring at younger ages and anyone with the symptoms - unusual bowel habits for three weeks or more, bleeding from the bottom and pains in the abdomen - should consult their GP and preferably have a colonoscopy,” says Barbara, who adds she was not offered a colonoscopy in February 2000 when she went to her doctor.
“We can do something to help ourselves and we need to take action. We are responsible for our own lives,” she stresses.









Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel